What If Everything You Were Told About Hormone Therapy Was Wrong? The Data That Changes Everything
Share on:
About this Podcast
Part 1 of 2: This episode breaks down the Women's Health Initiative study and why early estrogen intervention saves lives. Part 2 explores testosterone, advanced therapies, and complete hormone optimization.
The 2002 Women's Health Initiative study created mass fear around hormone replacement therapy that persists 23 years later. Millions of women were denied access to treatment that could have prevented breast cancer, heart attacks, strokes, Alzheimer's disease, osteoporosis, and metabolic dysfunction. The study used the wrong women at the wrong age with the wrong hormones delivered the wrong way. Media misinterpreted the results and created headlines that changed women's health forever.
On the Legacy and Longevity Podcast, COO Zach Dancel and Clinical Director Stephanie Misanik break down exactly what went wrong, why bioidentical hormone therapy started during perimenopause in the mid-thirties creates lifelong protection, and how the gender disparity in medicine leaves women with zero FDA-approved testosterone formulations while men have over 30. This conversation exposes the medical travesty that cost an entire generation their health and proves the science has always supported early hormone intervention for women.
What The Women's Health Initiative Got Wrong
The Women's Health Initiative tested hormone replacement therapy on women with an average age of 63. Most women reach menopause in their early to mid-fifties. By age 63, women are already 10 years past menopause. That timing matters enormously because once hormones decline and estrogen receptors downregulate, damage begins accumulating in arteries, brain tissue, and bone density that late intervention cannot fully reverse.
The study used synthetic hormones, including horse estrogen and synthetic progestins that come with significant side effects. Modern bioidentical hormone therapy uses hormones with molecular structures identical to what the human body produces naturally. When you introduce molecules into the body that don't match natural structure, inflammation increases and side effects multiply. Research on bioidentical versus synthetic hormones published in Climacteric shows that bioidentical formulations produce fewer adverse events and better patient-reported outcomes compared to synthetic alternatives.
The Women's Health Initiative administered hormones orally. Anything swallowed goes through the gastrointestinal tract and liver, which activates the clotting cascade and increases blood clot risk. Transdermal application through creams or subcutaneous pellets bypasses the liver, eliminates clotting risk, and provides better absorption. Oral hormones might deliver 10% absorption after processing through the digestive system. Pellets provide nearly 100% bio availability.
Wrong people, wrong hormones, wrong delivery method. Yet the media ran headlines that scared women away from treatment for over two decades.
Peri-menopause Starts In Your Mid-Thirties
Menopause officially occurs after 12 consecutive months without a menstrual period. That's the moment your ovaries completely shut down estrogen and progesterone production. But perimenopause, the transition leading to menopause, begins 10 to 15 years earlier in the mid to late thirties. Most people picture a woman in her fifties or sixties when they think of menopause. That misconception causes women to miss the critical intervention window.
Testosterone deficiency happens first in the early thirties before estrogen fluctuations begin. Brain fog, difficulty focusing, inability to remember schedules or where you placed your keys all start during perimenopause, not menopause. Weight gain around the midsection, difficulty building muscle, increased insulin resistance, and metabolic dysfunction begin when testosterone drops and estrogen starts fluctuating wildly.
Women in their mid-thirties go to doctors complaining of mood disturbances, weight gain, brain fog, and focus issues. The last discussion that happens involves hormonal balance. Data on ADHD diagnoses in women shows massive increases in middle-aged women receiving stimulant medication prescriptions. Is ADHD suddenly appearing in the forties, or is executive function declining due to testosterone and estrogen loss? The hormone explanation seems far more obvious than a sudden ADHD epidemic creating stimulant medication shortages.
Medical education stopped teaching hormone therapy after the Women's Health Initiative. Even if medical schools covered perimenopause and menopause phases, hormone therapy wasn't discussed. The knowledge gap causes providers to misdiagnose and mistreat women presenting with actual hormone imbalance as depression, anxiety, ADHD, and sleep disorders. Symptom management replaces root cause treatment.
The Timing Hypothesis Saves Lives
A study presented at the Menopause Society annual meeting analyzed over 120 million women who started estrogen therapy early versus during menopause. Women who started estrogen 10 years before menopause showed a 66% reduction in breast cancer, heart attacks, and strokes. This isn't new science. Researchers have known this for decades while millions of women were denied access to life-saving therapy based on a flawed study design and media fear campaign.
The timing hypothesis explains why early intervention matters. Estrogen receptors need an active hormonal environment to function properly. The longer your body goes without estrogen, the more those receptors downregulate and become less responsive. They lose their protective signaling capacity. Early hormone replacement therapy keeps receptors active and responsive to deliver cardiovascular protection, neuro-protection, bone protection, and metabolic benefits.
The KEEPS trial published in 2012 studied recently menopausal women, not women 10 years past menopause. The Kronos Early Estrogen Prevention Study used low-dose estrogen plus progesterone and found no increase in cardiovascular events. The study showed slower progression of atherosclerosis when intervention started early. Not only does early hormone therapy pose no cardiovascular risk, it actively slows one of the most common and deadly cardiovascular diseases.
The ELITE trial published in 2016 tested the timing hypothesis directly by comparing women who started estrogen within six years of menopause versus 10 years after menopause. The Early versus Late Intervention Trial with Estradiol confirmed that women who started earlier showed slower progression of carotid artery hardening and overall arterial aging. Earlier intervention provides cardiovascular protection that late intervention cannot replicate.
What The Estrogen-Only Arm Actually Showed
The Women's Health Initiative included one arm that received estrogen without progestin. Progesterone is only prescribed alongside estrogen for women with a uterus because estrogen builds the uterine lining. Without a menstrual period to shed that lining, tissue accumulation increases endometrial hyperplasia risk over time. Women who had hysterectomies received estrogen alone.
That estrogen-only arm showed results completely opposite to the fear narrative. Women taking estrogen alone demonstrated a 22% reduction in breast cancer incidence and a 40% reduction in breast cancer mortality compared to women taking no estrogen. Not only were they less likely to develop breast cancer, they were significantly less likely to die from it if diagnosed.
The data proving estrogen's protective benefits existed in the original study. Misinterpretation and media sensationalism created fear that persists today despite evidence showing the opposite. The main culprit causing problems in the Women's Health Initiative was the synthetic progestin, not the estrogen.
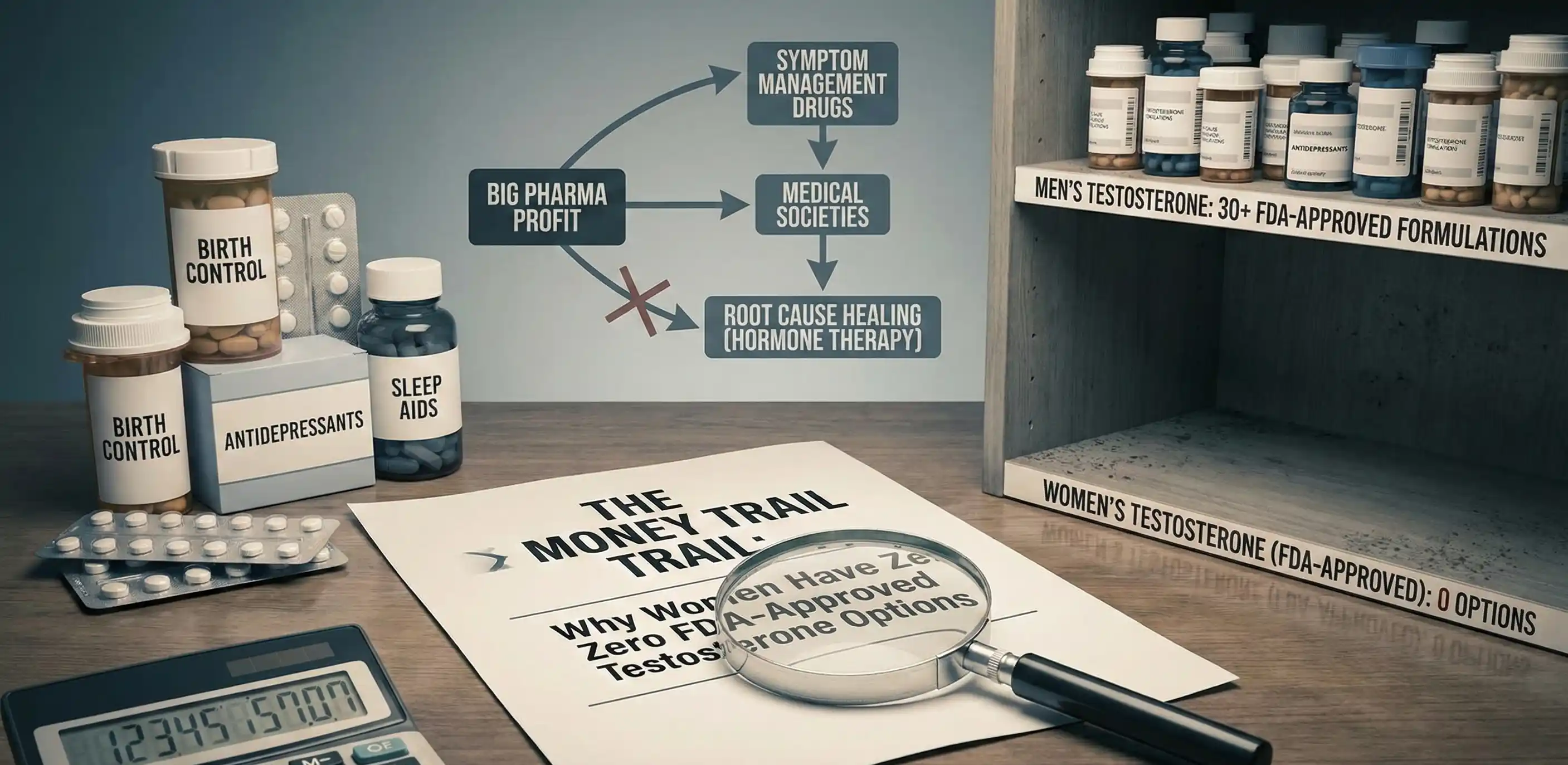
Gender Disparity In Medicine
If men slowly lost testosterone production throughout their 40s with no medical solutions available, pharmaceutical companies would mobilize immediately to create interventions. That's exactly what happens to women during perimenopause and menopause. Men receive over 30 FDA-approved testosterone formulations. Women have zero despite making up 52% of the population.
Sexual dysfunction solutions illuminate the disparity clearly. Men have 15 to 17 FDA-approved treatments including pills, creams, devices, and shockwave therapy. Some require significant pharmaceutical investment and extensive studies for FDA approval. Women have no FDA-approved sexual health solutions despite experiencing painful sex, vaginal dryness, chronic UTIs, and complete loss of libido during hormone decline.
Studies historically excluded women because female physiology is more complex and pregnancy during trials creates ethical issues. At some point, medical institutions must acknowledge that complexity doesn't justify complete exclusion. Women deserve solutions that match the investment men receive for comparable issues.
Find Experts Not Just Prescribers
Telemedicine platforms offering hormone prescriptions without comprehensive evaluation create safety concerns. Monitoring and treating hormones requires far more than shooting for a number on a lab panel. Providers who say they target a specific range without considering symptoms, hormone metabolism, detoxification pathways, nutrient status, and thyroid function don't understand hormone optimization.
Not all doctors know about hormones. Most endocrinologists are not hormone experts despite their title. Most OBGYNs receive surgical and procedural training, not hormone management education. Finding a provider with true expertise, experience, and knowledge to manage hormones safely and effectively requires research. Look for practitioners who trained outside medical school through organizations like the Institute for Functional Medicine or American Academy of Anti-Aging Medicine.
Hormone therapy used appropriately saves lives. Used inappropriately, it creates risks. This is medicine, not guesswork. Find experts who understand estrogen metabolism, detoxification pathways, how to manage side effects like estrogen dominance, and why thyroid must be addressed alongside sex hormones. Cookie-cutter protocols don't work. Precision personalized medicine based on your unique physiology, symptoms, and lab work produces optimal outcomes.
Rewriting Women’s Health Forever
The Women's Health Initiative cost millions of women their health by using the wrong study design and creating media-driven fear. The science always supported bioidentical hormone therapy started early during perimenopause in the mid-thirties. A study of 120 million women proves early intervention reduces breast cancer, heart attacks, and strokes by 66%. The timing hypothesis shows estrogen receptors need active hormonal environments to maintain protective functions. Late intervention after damage accumulates cannot replicate the benefits of early treatment.
If you're a woman experiencing brain fog, weight gain, mood changes, or focus issues in your thirties or forties, hormone imbalance is more likely than sudden ADHD or depression. Find a functional medicine provider with hormone expertise who will test comprehensively and treat root causes instead of managing symptoms with antidepressants and stimulants. Subscribe to the Legacy and Longevity Podcast wherever you listen and learn how to optimize hormones for lifelong health.
Discover how to align your biology with circadian rhythms and build a health span that matches your lifespan. Stop managing symptoms—start mastering your health with daily habits that transform your biology. Discover your path to peak health; to know more, click on the link below:
Follow Legacy and Longevity Podcast:
Website: LegacyandLongevity.com | Facebook: Legacy-and-Longevity-Podcast | YouTube: @LegacyandLongevityPodcast | Instagram: @LegacyandLongevity
Follow Zach Dancel:
Instagram: @ZachDancel | Facebook: Zach.Dancel | LinkedIn: @ZachDancel
Follow Stephanie Misanik:
LinkedIn: @SMHHC
Listen & Subscribe
Available on all major podcast platforms

 Spotify
Spotify
 Apple
Apple
 Amazon Music
Amazon Music
 Youtube
Youtube






Comments